Procedures

Slide title
Digital X-rays
Button
Slide title
Teeth Whitening
Button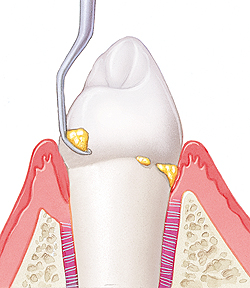
Slide title
Dental Cleaning
Button
Slide title
Cosmetic Fillings
Button
Slide title
Restorative Fillings
Button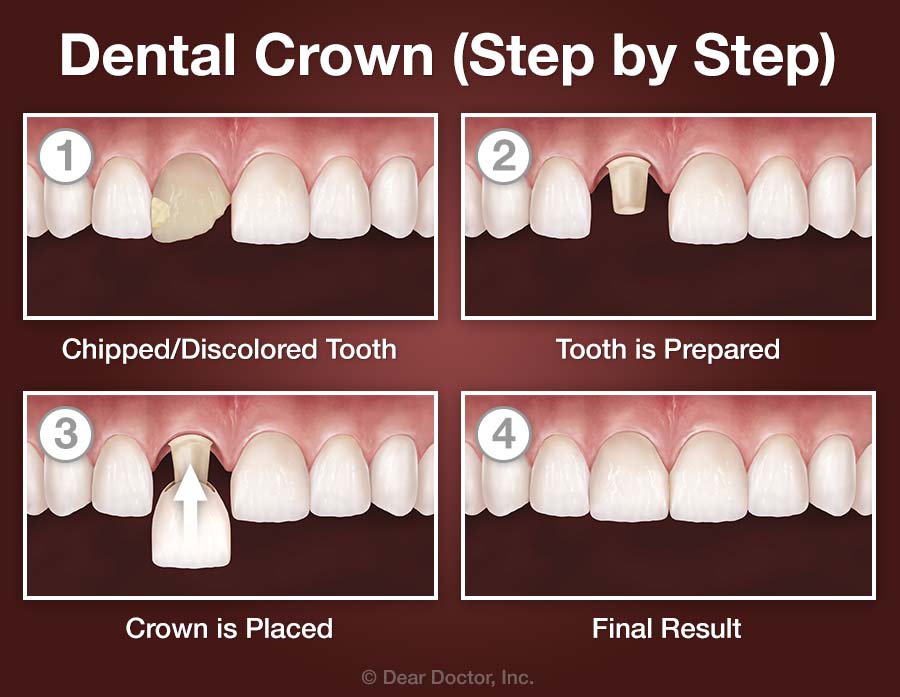
Slide title
Crown
Button
Slide title
Bridges
Button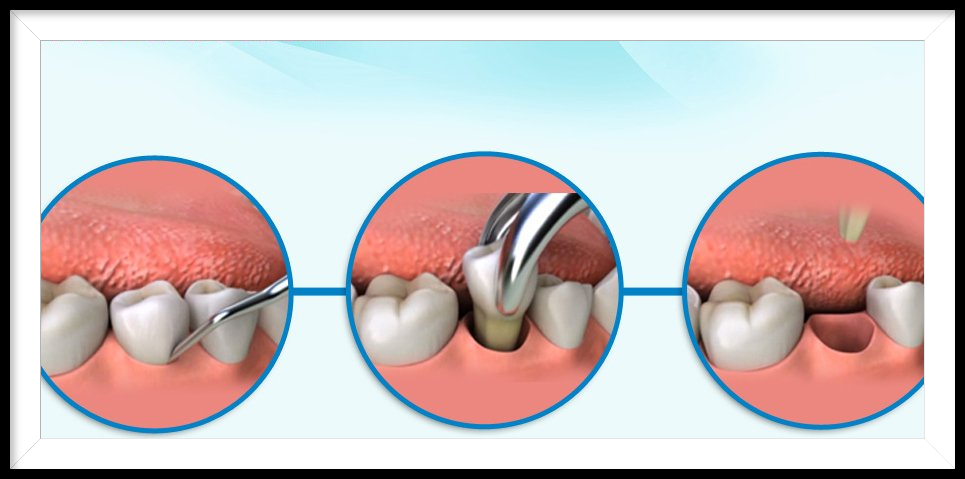
Slide title
Extractions
Button
Slide title
Bone Grafting
Button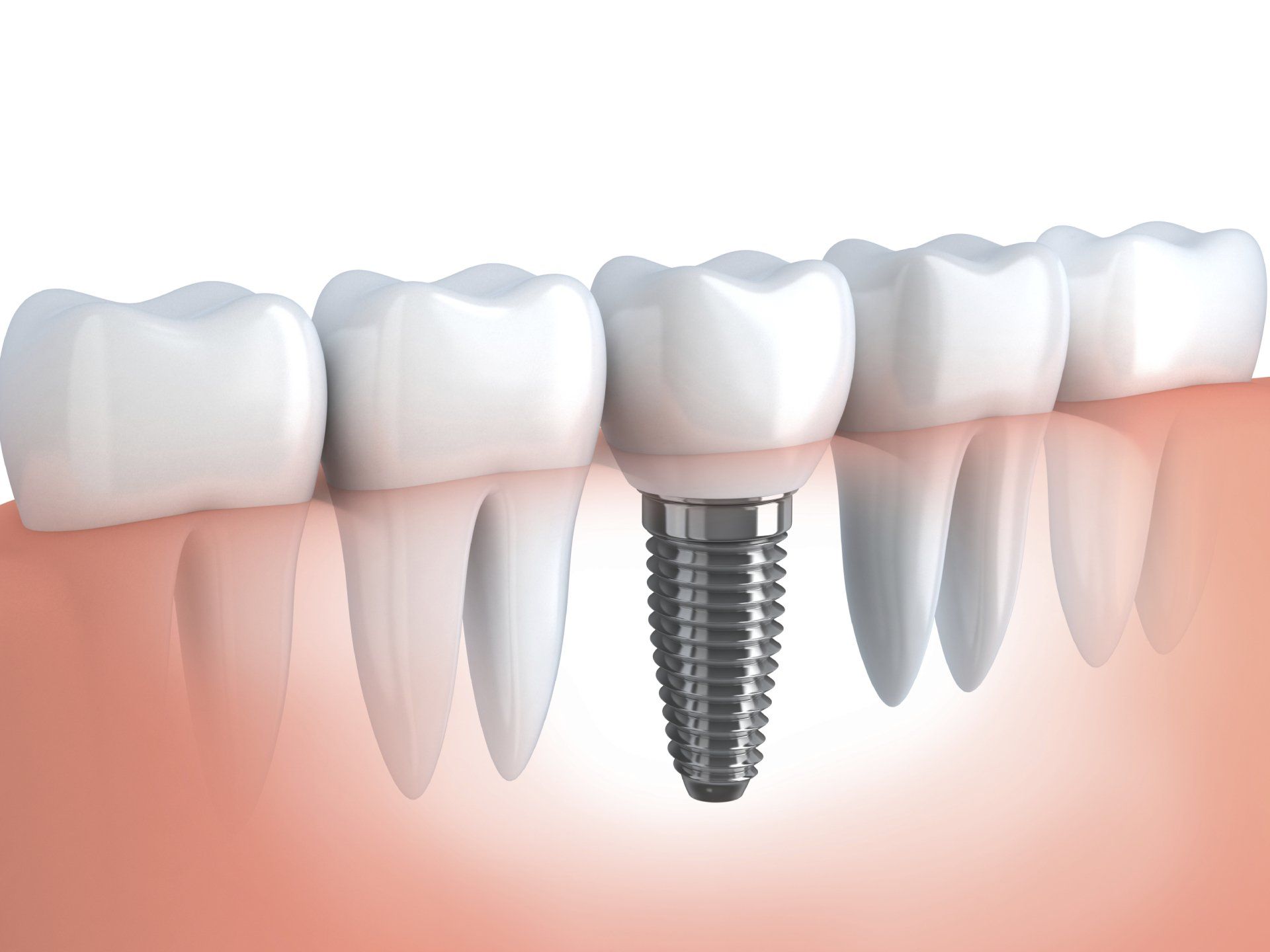
Slide title
Dental Implants
Button
Slide title
Dentures
Button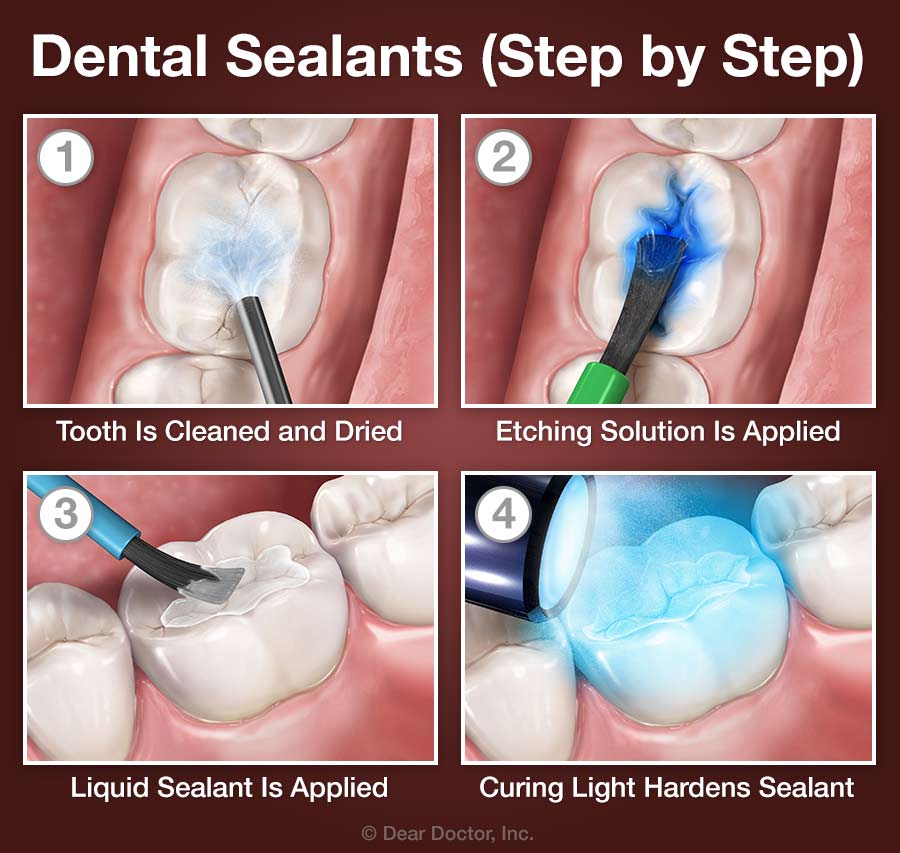
Slide title
Sealants
Button
- Digital Xrays
Digital radiography (digital X-ray) is the latest technology used to take dental X-rays. This technique uses an electronic sensor (instead of X-ray film) that captures and stores the digital image on a computer. This image can be instantly viewed and enlarged, helping the dentist and dental hygienist detect problems more easily. Digital X-rays reduce radiation 80-90% compared to the already low exposure of traditional dental X-rays.
Dental X-rays are essential preventative and diagnostic tools that provide valuable information not visible during a clinical dental exam. Dentists and dental hygienists use this information to safely and accurately detect dental abnormalities to provide an accurate treatment plan. Without X-rays, problem areas can go undetected.
Dental X-rays may reveal:
--Abscesses or cysts.
--Bone loss.
--Cancerous and non-cancerous tumors.
--Decay between the teeth.
--Developmental abnormalities.
--Poor tooth and root positions.
--Problems inside a tooth or below the gum line.
--Detecting and treating dental problems at an early stage can save you time, money, unnecessary discomfort, and your teeth!
Are dental X-rays safe?
We are all exposed to natural radiation in our environment. Digital X-rays produce a significantly lower level of radiation compared to traditional dental x-rays. Not only are digital X-rays better for the health and safety of the patient, they are faster and more comfortable to take, which reduces your time in the dental office.
Even though digital X-rays produce a low level of radiation and are considered very safe, dentists still take necessary precautions to limit the patient’s exposure to radiation. These precautions include only taking those X-rays that are necessary, and using lead apron shields to protect the body.
How often should dental X-rays be taken?
The need for dental X-rays depends on each patient’s individual dental health needs. Your dentist and dental hygienist will recommend necessary X-rays based upon the review of your medical and dental history, a dental exam, signs and symptoms, your age, and risk of disease.
A full mouth series of dental X-rays is recommended for new patients. A full series is usually good for three to five years. Bite-wing X-rays (X-rays of top and bottom teeth biting together) are taken at recall (check-up) visits and are recommended once or twice a year to detect new dental problems.
- Teeth Whitening
Teeth whitening (or bleaching) is a simple, non-invasive dental treatment used to change the color of natural tooth enamel and is an ideal way to enhance the beauty of your smile.
Because having whiter teeth has now become the number one aesthetic concern of most patients, there are a number of ways to whiten teeth. The most popular method is using a home teeth whitening system that will whiten teeth dramatically. Since teeth whitening only works on natural tooth enamel, it is important to evaluate replacement of any old fillings, crowns, etc. Replacement of any restorations will be done after bleaching so they will match the newly bleached teeth.
Teeth whitening is not permanent. A touch-up may be needed every several years, and more often if you smoke, drink coffee, tea, or wine.
What does teeth whitening involve?
This type of teeth whitening usually requires two visits. At the first appointment, impressions (molds) will be made of your teeth to fabricate custom, clear, plastic, trays.
At your second visit, you may pick up your bleaching trays and the bleaching tubes.
The trays are worn with special whitening solution either twice a day for 30 minutes or overnight for a couple of weeks depending on the degree of staining and desired level of whitening. It is normal to experience tooth sensitivity during the time you are whitening your teeth, but it will subside shortly after you have stopped bleaching.
You will receive care instructions for your teeth and trays, and be encouraged to visit your dentist regularly to help maintain a beautiful, healthy, white smile.
- Dental Cleaning
Professional dental cleanings (dental prophylaxis) are performed by Registered Dental Hygienists. Your cleaning appointment will include the following:
- Removal of calculus (tartar): Calculus is hardened plaque that has been left on the tooth for some time and is now firmly attached to the tooth surface. Calculus forms above and below the gum line and can only be removed with special dental instruments.
- Removal of plaque: Plaque is a sticky, almost invisible film that forms on the teeth. It is a growing colony of living bacteria, food debris, and saliva. The bacteria produce causes inflammation of the gingiva. This inflammation is the start of periodontal disease!
- Teeth polishing: Remove stain and plaque that is not otherwise removed during tooth brushing and scaling.
Our hygienists will educate you on your specific oral and periodontal conditions. You may have to make subsequent appointments due to any periodontal disease conditions for optimum treatment.
- Cosmetic and Restorative Filliings
COSMETIC BONDING/FILLINGS:
Bonding is a cosmetic procedure that allows the dentist to reshape or repair your smile using composite resin. Cosmetic bonding is particularly ideal if you’re insecure about the appearance of your smile. With bonding, chipped or uneven teeth can be repaired easily and affordably, restoring your self-confidence. Additionally, bonding is often completed in a single visit.
As with most cosmetic procedures, bonding will wear and discolor over time, eventually needing to be replaced; however, bonding is very durable and typically lasts many years.
Reasons for cosmetic bonding:
- Closing spaces or gaps
- Fixing chipped teeth
- Fixing decayed teeth (teeth with cavities)
- Lengthening uneven teeth
- Protecting roots exposed by receding gums
- Restoring badly discolored teeth
RESTORATIVE FILLINGS:
Restorative fillings are needed when part of the tooth structure has decayed due to bacteria not being brushed and flossed away properly.
If the bacteria advances too far into the tooth, it will reach the nerve and will need a root canal. In some cases, the decay is too advanced and the tooth is non-restorable resulting in extraction.
For restorative fillings, we use a variety of materials. If you have specific concerns about certain materials, please address them with Dr. Strupp.
Dr. Strupp will help you understand your options with tooth decay and what will work best for your specific mouth and oral conditions.
- Crowns/Bridges
CROWNS:
A crown (or cap) is a covering that encases the entire tooth surface restoring it to its original shape and size. A crown protects and strengthens tooth structure that cannot be restored with fillings or other types of restorations.
Reasons for crowns:
- Broken or fractured teeth
- Cosmetic enhancement
- Decayed teeth
- Fractured/large fillings
- Tooth has a root canal
What does getting a crown involve?
A crown procedure requires two appointments. Your first appointment will include taking several highly accurate molds (or impressions) that will be used to create your custom crown. A mold will also be used to create a temporary crown which will stay on your tooth for approximately three weeks until your new crown is fabricated by a dental laboratory.
While the tooth is numb, the dentist will prepare the tooth by removing any decay and shaping the surface to properly fit the new crown. Once these details are accomplished, your temporary crown will be placed with temporary cement and your bite will be checked to ensure proper occlusion.
At your second appointment your temporary crown will be removed, the tooth will be cleaned, and your new crown will be carefully placed to ensure the contacts between other teeth and bite are accurate.
There are a couple different crown materials to choose from, including tooth colored crowns and gold crowns.
BRIDGES:
A dental bridge is a fixed (non-removable) appliance and is an excellent way to replace missing teeth.
There are several types of bridges. You and your dentist will discuss the best options for your particular case. A bridge consists of two crowns that go over two anchoring teeth (abutment teeth) and are attached to pontics (artificial teeth), filling the gap created by one or more missing teeth.
Dental bridges are highly durable and will last many years; however, they may need replacement or need to be re-cemented due to normal wear.
Reasons for a fixed bridge:
- Fill space of missing teeth
- Prevent remaining teeth from drifting out of position
- Restore chewing and speaking ability
- Restore your smile
What does getting a fixed bridge involve?
Getting a bridge usually requires two or more visits. While the teeth are numb, the two anchoring teeth are prepared by removing a portion of enamel to allow for a crown. Next, a highly accurate impression (mold) is made which will be sent to a dental laboratory where the bridge will be fabricated. In addition, a temporary bridge will be made and worn for several weeks until your next appointment.
Next, your permanent bridge will be carefully checked, adjusted, and cemented to achieve a proper fit.
You will receive care instructions at the conclusion of your treatment. Proper brushing, flossing and regular dental visits will aid in the life of your new permanent bridge.
- Extractions
If you are experiencing extreme sensitivity or pain or are suffering from advanced periodontal disease, you may be required to have a tooth extracted. With a simple extraction, the dentist can safely remove the affected tooth without the need for major surgery.
Reasons for a tooth extraction:
There are numerous situations in which an extraction can help alleviate pain or prepare you for another cosmetic or restorative procedure.
Some common reasons for extraction include:
- Advanced periodontal disease that has loosened the tooth roots
- Extra teeth or baby teeth that impede adult teeth
- Preparing a patient for orthodontic treatment
- Removing a fractured or malformed tooth
- Severe tooth decay which cannot be remedied with root canal therapy
What to expect after an extraction:
Once the local anesthetic wears off, you may experience some discomfort. This pain subsides a little more each day. Depending on the tooth and individual circumstances, you may need to take medication following a tooth extraction. Dr. Strupp will discuss post-op care with you.
Tooth extractions carry a risk of dry socket. This means the blood clot at the extractions site gets removed and exposes the bone underneath. It is painful, but can be remedied fairly quickly. After an extraction, if you experience more pain the fourth day than the first, and the pain radiates in to the jaw and sometimes to the ear area, you may have a dry socket. Please contact our office if this happens.
POST OP INSTRUCTIONS FOR EXTRACTIONS:
- Please do not smoke, drink hot drinks, or drink alcohol
- Do not suck out of a straw
- Do not eat popcorn or hard/sticky candies
- Do not spit or rinse vigorously
- Keep pressure on gauze for 30-90 minutes after extraction
- Eat soft foods
- Rinse carefully with warm salt water after 12 hours, but do not forcefully spit it out--let it fall out of your mouth into sink
- Please take any prescribed medication
- Call our office with any other quesitons
WISDOM TEETH EXTRACTIONS:
Third molars, commonly referred to as wisdom teeth, are usually the last four of 32 teeth to erupt in the mouth, generally making their appearance between the ages of 17 to 25. They are located at the back of the mouth (top and bottom/left and right). The term “wisdom” stems from the idea that the molars surface at a time typically associated with increased maturity or “wisdom”.
In most cases, inadequate space in the mouth does not allow the wisdom teeth to erupt properly and become fully functional. When this happens, the tooth can become impacted (stuck) in an undesirable or potentially harmful position. If left untreated, impacted wisdom teeth can contribute to infection, damage to other teeth, and possibly cysts or tumors.
There are several types, or degrees, of impaction based on the actual depth of the teeth within the jaw:
- Soft Tissue Impaction: The upper portion of the tooth (the crown) has penetrated through the bone, but the gingiva (gum) is covering part or all of the tooth’s crown and has not positioned properly around the tooth. Because it is difficult to keep the area clean, food can become trapped below the gum and cause an infection and/or tooth decay, resulting in pain and swelling.
- Partial Bony Impaction: The tooth has partially erupted, but a portion of the crown remains submerged below the gum and surrounding jawbone. Again, because it is difficult to keep the area clean, infection will commonly occur.
- Complete Bony Impaction: The tooth is completely encased by jawbone. This will require more complex removal techniques.
Reasons to remove wisdom teeth
While not all wisdom teeth require removal, wisdom teeth extractions are most often performed because of an active problem such as pain, swelling, decay or infection, or as a preventative measure to avoid serious problems in the future. If impaction of one or more wisdom teeth is present, and left untreated, a number of potentially harmful outcomes can occur, including:
- Damage to nearby teeth: Second molars (the teeth directly in front of the wisdom teeth) can be adversely affected by impacted wisdom teeth, resulting in tooth decay (cavities), periodontal disease (gum disease) and possible bone loss.
- Disease: Although uncommon, cysts and tumors can occur in the areas surrounding impacted wisdom teeth.
- Infection: Bacteria and food can become trapped under the gum tissue, resulting in an infection. The infection can cause considerable pain and danger.
- Tooth Crowding: It has been theorized that impacted wisdom teeth can put pressure on other teeth and cause them to become malaligned (crowded or twisted). This theory isn’t universally accepted by all dental professionals, and it has not been validated by scientific studies.
Wisdom teeth examination
As with any dental procedure, your dentist will want to initially conduct a thorough examination of the wisdom and surrounding teeth. Panoramic digital X-rays will be taken in order for your dentist to evaluate the position of the wisdom teeth and determine if a current problem exists, or the likelihood of any potential future problems. The X-rays can also expose additional risk factors, such as deterioration or decay of nearby teeth.
Early evaluation and treatment (typically in the mid-teen years) is recommended in order to identify potential problems and to improve the results for patients requiring wisdom teeth extractions. Only after a thorough examination can your dentist provide you with the best options for your particular case. In some cases, referral to an oral surgeon may be necessary.
- Bone Grafting
The bone grafting procedure is an excellent way to replace lost bone tissue and encourage natural bone growth. Bone grafting is a versatile and predictable procedure which fulfills a wide variety of functions.
A bone graft may be required to create a stable base for dental implant placement, to halt the progression of gum disease, or to make the smile appear more aesthetically pleasing.
There are a wide variety of reasons why bone grafting may be the best option for restoring areas of the mouth.
- Dental implants – Implants are the preferred replacement method for missing teeth because they restore full functionality to the mouth; however, implants need to be firmly anchored to the jawbone to be effective. If the jawbone lacks the necessary quality or quantity of bone, bone grafting can strengthen and thicken the implant site.
- Sinus lift – A sinus lift elevates the sinus membrane and grafting bone onto the sinus floor so that implants can be securely placed.
- Ridge augmentation – Ridges in the bone can occur due to trauma, injury, birth defects, or severe periodontal disease. The bone graft is used to fill in the ridge and make the jawbone a uniform shape.
What does bone grafting treatment involve?
Bone grafting is generally a procedure that can be performed under local anesthetic; however, if large amounts of bone area need to be grafted, general anesthetic may be required.
Initially, the grafting material needs to either be harvested or prepared for insertion. We generally perform bone grafts after an extraction, when an implant is planned to replace that tooth. The bone grafting material is placed at the affected site directly after the extraction.
- Dental Implants
Dental implants are a great way to replace missing teeth and can also provide retention to dentures.
Dental implants are artificial roots and teeth (usually titanium) that are surgically placed into the upper or lower jaw bone by a general dentist, periodontist, endodontist, or oral surgeon.
Dental implants are strong, durable, natural looking and will last many years. On occasion, they will have to be re-tightened or replaced due to normal wear.
Reasons for dental implants:
- Replace one or more missing teeth without affecting adjacent teeth
- Resolve joint pain or bite problems caused by teeth shifting into missing tooth space
- Restore a patient’s confident smile
- Restore chewing and speech
- Restore or enhance facial profile
- Support a bridge or denture, making it more secure and comfortable.
What does getting dental implants involve?
The process of getting implants requires a number of visits over several months.
X-rays, bone scans and impressions (molds) are taken of the jaw and teeth to determine bone, gum tissue, and spacing available for an implant.
While the area is numb, the implant will be surgically placed into the bone and allowed to heal and integrate itself from four to six months. Depending on the type of implant, a second surgery may be required in order to place the “post” that will hold the artificial tooth in place.
After several weeks of healing the artificial teeth are made and fitted to the post portion of the anchor. Because several fittings may be required, this step may take one to two months to complete. After a healing period, the artificial teeth are securely attached to the implant, providing excellent stability and comfort to the patient.
You will receive care instructions when your treatment is completed. Good oral hygiene and eating habits, alongside regular dental visits, will aid in the life of your new implant.
- Dentures
Full or partial tooth loss may affect a person's self-image and can also increase the risk of developing nutritional problems and other health disorders. There's a way to treat this: full or partial dentures.
Dentures are just one option for replacing missing teeth; some of the others include fixed bridgework and dental implants. Each method has its particular pros and cons, which should be carefully considered. There are also several varieties of dentures available to address specific issues, from partial dentures to implant-supported overdentures. The best option for you will depend on your individual situation.
How Do Removable Dentures Work?
Full or partial dentures consist of a gum-colored base made of plastic resin, which fits over the remaining alveolar (bone) ridge that formerly held the teeth. The prosthetic teeth projecting from the base are designed to look and function just like your natural teeth. Dentures are held in place primarily by the suctioning effect of their close fit against the alveolar ridges — that's why it's so important that they are fitted properly. The upper denture also gets extra support from the large surface area of the roof of the mouth (palate), which helps makes it stable.
At first, wearing dentures may require some getting used to in terms of talking and eating. But over time, the muscles, nerves and ligaments of the mouth learn to work in new ways, which allows these functions to occur normally. Dentures also help support the facial skeleton and the soft tissues of the lips and cheeks, which can help create a more youthful appearance.
Types of Full Dentures
Removable denture types:
- Immediate Dentures: These are usually a temporary means of helping you transition to successful denture wearing. Because of the muscular readjustment required, as well as the natural shrinkage of gums, the dentures which are placed immediately after tooth extraction won't fit as well as permanent dentures made when the healing is complete. They do, however, provide you with new teeth right away, and give you time to adjust.
- Conventional Full Dentures: After a period of time, permanent dentures that conform to your mouth more fully can be fabricated. These are carefully crafted to look like natural teeth, and are able to function properly in your mouth for a long time.
- Implant-Supported Overdentures: To increase the stability of a lower or upper denture, it's possible for them to be securely anchored using two or more dental implants. The upper jaw requires more implants (generally three or more) than the lower jaw due to a lesser bone density. Many people find this option offers a greater balance of comfort, functionality and value.
Types of Partial Dentures
- Transitional Partial Dentures (Flipper): These relatively inexpensive removable plastic dentures serve as a temporary tooth replacement and space maintainer as you wait for your mouth to heal from tooth extraction, for example. Once the healing process is complete, dental implants can be placed.
- Removable Partial Dentures (RPDs): Usually made of cast vitallium, these well-constructed, metal-based removable partial dentures are much lighter and less obtrusive than those made of plastic. They are a little more expensive than plastic dentures but will fit better. They are less expensive than implants or fixed bridgework.
How Dentures Are Made and Fitted
Making quality dentures is a blend of science and art. First, an accurate impression (mold) is made of the alveolar ridges on the top and bottom of your mouth. The base of the denture is made from this mold in a dental laboratory. Working together, the dentist and lab technician choose from among many different sizes and shapes of prosthetic teeth to re-create a natural-looking smile. When everyone is satisfied with the result, the temporary dentures are made in permanent form.
To enable normal speech and eating, it's crucial to balance your bite. This means that the upper and lower dentures come together and properly stabilize each other. The form and function of the dentures are carefully checked to ensure that they are working and fitting properly.
What to Expect After You Get Dentures
If you've recently lost your teeth and received an immediate denture, it's normal to find some tissue shrinkage and bone loss occurring. Therefore, in several months you may find that your immediate dentures no longer fit well. You will have two choices at this point: You can have your immediate (temporary) dentures re-lined. This means that material is added under the denture's base to better conform to the new contours of your alveolar ridge. Another option is to move to a set of conventional full dentures, which will last longer and fit better. With proper care, dentures offer a functional, aesthetic and economical solution to the problem of tooth loss.
- Sealants
The most likely place for a cavity to develop in your child's mouth is on the chewing surfaces of the back teeth. These surfaces are not smooth, as other areas of your teeth are. Instead, they are filled with tiny grooves referred to as “pits and fissures,” which trap bacteria and food particles. The bristles on a toothbrush can't always reach all the way into these crevices.
A child's newly erupted permanent teeth are not as resistant to decay as adult teeth are. The hard enamel coating that protects the teeth changes as it ages to become stronger. Fluoride, which is found in toothpaste and some drinking water — and in treatments provided at the dental office — strengthens enamel, but, again, it's hard to get fluoride into those pits and fissures on a regular basis. Fortunately, there is a good solution to this problem: dental sealants.
Dental sealants are invisible plastic resin coatings that smooth out the chewing surfaces of the back teeth, making them resistant to decay. A sealed tooth is far less likely to develop a cavity, require more expensive dental treatment later on, or, most importantly, cause your child pain.
How Sealants Are Placed
You can think of a sealant as a mini plastic filling, though please reassure your child that it doesn't “count” as having a cavity filled. Because tooth enamel does not contain any nerves, placing a sealant is painless and does not routinely require numbing shots.
First, the tooth or teeth to be sealed are examined, and if any minimal decay is found, it will be gently removed. The tooth will then be cleaned and dried. Then a solution that will slightly roughen or “etch” the surface is applied, to make the sealing material adhere better. The tooth is then rinsed and dried again. The sealant is then painted on the tooth in liquid form and hardens in about a minute, sometimes with the help of a special curing light. That's all there is to it!
Taking Care of Sealants
Sealed teeth require the same conscientious dental hygiene as unsealed teeth. Your child should continue to brush and floss his or her teeth daily and have regular professional cleanings. Checking for wear and tear on the sealants is important, though they should last for up to 10 years. During this time, your child will benefit from a preventive treatment proven to reduce decay by more than 70 percent.